Guidelines
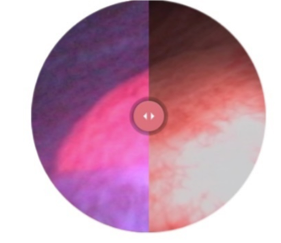
Blue Light Cystoscopy (BLC®) with Cysview® is included in U.S. and international industry guidelines. These key industry organizations acknowledge the clinical value of this leading-edge drug-device technology.
Diagnosis and Treatment of Non-Muscle Invasive Bladder Cancer: AUA/SUO Joint Guideline 2016 (Amended 2020)1
The American Urological Association and the Society of Urologic Oncology included this statement in their 2016 guideline (amended 2020).
#30. In a patient with NMIBC, a clinician should offer blue light cystoscopy at the time of TURBT, if available, to increase detection and decrease recurrence. (Moderate Recommendation; Evidence Strength: Grade B)
Cysview may not detect all malignant lesions. False-positive fluorescence may occur due to inflammation, cystoscopic trauma, scar tissue, previous bladder biopsy, recent BCG immunotherapy or intravesical chemotherapy.
Cysview is not a replacement for random biopsies or other procedures used in the detection of bladder cancer. Please see Full Prescribing Information.
For more information review the Important Risk & Safety Information at the bottom of this page.
Guideline Statements
Diagnosis
- At the time of resection of suspected bladder cancer, a clinician should perform a thorough cystoscopic examination of a patient’s entire urethra and bladder that evaluates and documents tumor size, location, configuration, number, and mucosal abnormalities. (Clinical Principle)
- At initial diagnosis of a patient with bladder cancer, a clinician should perform complete visual resection of the bladder tumor(s), when technically feasible. (Clinical Principle)
- A clinician should perform upper urinary tract imaging as a component of the initial evaluation of a patient with bladder cancer. (Clinical Principle)
- In a patient with a history of NMIBC with normal cystoscopy and positive cytology, a clinician should consider prostatic urethral biopsies and upper tract imaging, as well as enhanced cystoscopic techniques (blue light cystoscopy, when available), ureteroscopy, or random bladder biopsies. (Expert Opinion)
Risk Stratification
- At the time of each occurrence/recurrence, a clinician should assign a clinical stage and classify a patient accordingly as “low-,” “intermediate-,” or “high-risk.” (Moderate Recommendation; Evidence Strength: Grade C)
| AUA Risk Stratification for Non-Muscle Invasive Bladder Cancer | ||
|---|---|---|
| Low Risk | Intermediate Risk | High Risk |
| LGa solitary Ta ≤ 3cm | Recurrence within 1 year, LG Ta | HG T1 |
| PUNLMPb | Solitary LG Ta > 3cm | Any recurrent, HG Ta |
| LG Ta, multifocal | HG Ta, >3cm (or multifocal) | |
| HGc Ta, ≤ 3cm | Any CISd | |
| LG T1 | Any BCG failure in HG patient | |
| Any variant histology | ||
| Any LVIe | ||
| Any HG prostatic urethral involvement | ||
| aLG = low grade; bPUNLMP = papillary urothelial neoplasm of low malignant potential; cHG = high grade; dCIS=carcinoma in situ; eLVI = lymphovascular invasion |
||
National Comprehensive Cancer Network Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Bladder Cancer (Updated 2021)2
The NCCN Guidelines state in the Principles of Surgical Management section for TURBT:
Enhanced cystoscopy may be helpful in identifying lesions not visible using white light cystoscopy.
Consider enhanced cystoscopy (if available) for initial evaluation or when positive urine cytology.
1 American Urological Association/Society of Urologic Oncology Non-Muscle Invasive Bladder Cancer Guideline 2016. https://www.auanet.org/guidelines/bladder-cancer-non-muscle-invasive-(2016)#x2572. Published 2016. Accessed January 17, 2019
2 Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines® ) for Bladder Cancer. Version 3.2021. © National Comprehensive Cancer Network, Inc. 2021. All rights reserved. Accessed April 26, 2021. To view the most recent and complete version of the guidelines, go online to NCCN.org. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way.


